IMMUNOTHERAPY
Latest News

Latest Videos

More News

The anti-PD-1 antibody pembrolizumab produced broad and durable responses in patients with recurrent/metastatic head and neck squamous cell carcinoma.

MPDL3280A reduced the risk of death by 53% compared with docetaxel in previously treated patients with PD-L1-positive squamous and non-squamous non-small cell lung cancer.
Immune checkpoint inhibition will continue to attract interest at the 2015 ASCO Annual Meeting, with a number of abstracts focused on this emerging class of agents

Gary D. Steinberg, MD, Bruce and Beth White Family Professor, professor of surgery, director, urologic oncology, University of Chicago Medicine, discusses the impact immunotherapy has had on bladder cancer.

Treatment with the PD-1 inhibitor nivolumab demonstrated similar efficacy regardless of prior treatment with a BRAF inhibitor or ipilimumab in patients with BRAF mutant or wild type metastatic melanoma.

Optimal outcomes, and perhaps even a cure, could be achieved with the combination of targeted therapies and immune checkpoint inhibitors.
Two presentations at this year’s American Association for Cancer Research (AACR) annual meeting linked a specific microRNA (miRNA), miR-34a, to an active area in immunotherapy, programed cell death-1 (PD-1) protein and its ligand, PD-L1.

Treatment with the PD-1 inhibitor nivolumab was active and tolerable across three doses for patients with metastatic renal cell carcinoma.

The PD-1 inhibitor nivolumab (Opdivo) has been has been assigned priority review designation from the US Food and Drug Administration (FDA) as a treatment for previously untreated patients with unresectable or metastatic melanoma.

MedImmune Limited, a subsidiary of AstraZeneca PLC, and Celgene International II Sà rl, a subsidiary of Celgene Corporation, have formed a strategic collaboration for the development and commercialization of AstraZeneca’s anti-programmed cell death-ligand 1 (PD-L1) agent MEDI4736.
Despite their promise, checkpoint inhibitors are not effective in every patient, and research suggests the STING (stimulator of interferon genes) pathway may hold important clues as to why some tumors fail to respond.

Mark R. Middleton, MD, PhD, discusses the results of a phase I/IIa trial of IMCgp100, a bispecific immunotherapy, for the treatment of patients with melanoma.
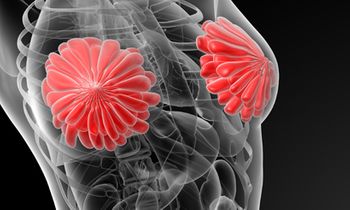
The PD-L1 inhibitor MPDL3280A demonstrated a 19% objective response rate (ORR) with 75% of responses ongoing in pretreated patients with metastatic triple-negative breast cancer (TNBC).
Results from the phase II, double-blind CheckMate-069 clinical trial showed unprecedented response rates with ipilimumab combined with nivolumab in previously treated patients with metastatic melanoma.

Jeffrey S. Weber, MD, PhD, a senior member at Moffitt Cancer Center, discusses toxicities associated with immunotherapies for the treatment of patients with melanoma.

Pembrolizumab (Keytruda) achieved an overall response rate (ORR) of 45.2% among a cohort of patients with high PD-L1-expressing non–small cell lung cancer (NSCLC) in the phase I KEYNOTE-001 trial.
Pembrolizumab (Keytruda) yielded significantly better outcomes compared with ipilimumab (Yervoy) in a randomized phase III trial of patients with advanced melanoma.

IMCgp100, an anti-CD3 antibody fragment fused to a gp100-specific T cell receptor, yielded long-lasting responses in patients with advanced melanoma.

Kevin B. Kim, MD, medical oncology, California Pacific Medical Center, discusses the outlook for T-VEC for the treatment of patients with melanoma.

Novel combinations and immunotherapies have significantly expanded treatment options for myeloma. Numerous studies, including the ASPIRE and ELOQUENT-2 trials, have shown positive results for triple drug combinations.

A 2:1 open-label phase II trial of the FANG vaccine achieved a marked delay in time to progression, in all 14 of 21 patients with stage III/IV ovarian cancer who participated. The other 7 patients did not receive the vaccine.
A trial comparing frontline pembrolizumab with ipilimumab for the treatment of advanced melanoma has met its progression-free survival (PFS) and overall survival (OS) endpoints and will be stopped early.

Immunotherapy vaccine approaches that involve harvesting a patient’s dendritic cells and priming them to recognize a tumor-specific antigen before injecting them back into the patient to activate a T-cell response against the tumor have achieved encouraging but limited success.

Heather Wakelee, MD, associate professor of medicine, oncology division, Stanford University, discusses the rationale for immunotherapy in non-small cell lung cancer (NSCLC).
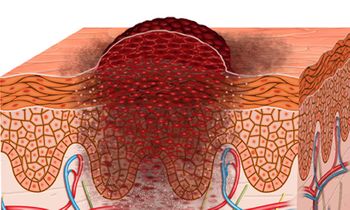
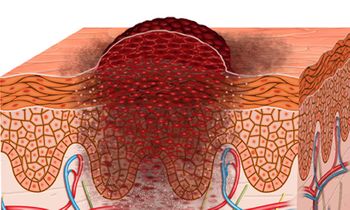
Cancer proliferates when a rogue, transformed cell wins a sophisticated hide-and-seek game against the immune system. Immunotherapy activates the patient’s immune system to recognize and fight the tumor cells.