Panelists discuss the TRIANGLE study, examining the efficacy and safety of the combination of rituximab, lenalidomide, and chemotherapy in treating high-risk diffuse large B-cell lymphoma and its potential to improve patient outcomes.
Panelists discuss the TRIANGLE study, examining the efficacy and safety of the combination of rituximab, lenalidomide, and chemotherapy in treating high-risk diffuse large B-cell lymphoma and its potential to improve patient outcomes.
Panelists discuss the inMIND study, exploring the efficacy and safety of mindetuximab for the treatment of relapsed or refractory non-Hodgkin lymphoma and its potential impact on future therapeutic strategies.
Panelists discuss the findings from the POLARIX study, focusing on the efficacy and safety of polatuzumab vedotin in combination with rituximab and chemotherapy for untreated diffuse large B-cell lymphoma.

Panelists discuss how health care providers can optimize quality-of-life and treatment outcomes for patients with myelofibrosis through comprehensive symptom management, shared decision-making, and careful attention to patient goals and expectations.

Panelists discuss how myelofibrosis progresses from its molecular and genetic origins through various clinical manifestations, ultimately informing the development of targeted therapeutic approaches for this bone marrow disorder.

The panelist discusses how real-world evidence for CAR T in relapsed/refractory multiple myeloma shows promising efficacy but with some differences from clinical trials. Ide-cel demonstrates effectiveness in patients with prior BCMA exposure, though responses may be impacted. Compared with standard of care (SOC), both ide-cel and cilta-cel show superior outcomes in terms of response rates and progression-free survival, though long-term data are still emerging in real-world settings.

The panelist discusses how the KarMMa-3 trial data demonstrated the superior efficacy of ide-cel vs standard regimens in triple-class exposed R/R MM, with a median progression-free survival of 13.3 vs 4.4 months and an overall response rate of 71% vs 42%. The favorable safety profile and significant survival benefit support ide-cel as a preferred option for third-line and greater treatment, particularly in patients with good performance status who can tolerate bridging therapy.

Panelists discuss how to optimize treatment selection and sequencing for a 65-year-old patient with standard-risk, transplant-eligible newly diagnosed multiple myeloma (NDMM) through assessment of disease characteristics, patient factors, and available therapeutic options.

Thomas W. LeBlanc, MD, MA, discusses how treatment regimens for low-risk myelodysplastic syndromes (LR-MDS) significantly impact health-related quality of life (HRQOL), with data from the COMMANDS study (Oliva et al, ASH 2024, Abstract 3216) highlighting the correlation between HRQOL and clinical end points, and explore how incorporating HRQOL data into clinical decision-making can guide more patient-centered treatment choices in community settings.

Panelists discuss how the IMROZ trial demonstrated improved outcomes with quadruplet therapy combining daratumumab, lenalidomide, melphalan, and prednisone in patients with transplant-ineligible newly diagnosed multiple myeloma (NDMM), highlighting its potential as a new treatment standard.

Panelists discuss the future treatment landscape for early relapsed/refractory multiple myeloma, emphasizing the evolving role of community providers, the implications for patient access to care, and how emerging data will influence treatment sequencing in subsequent lines of therapy.

Evan Y. Yu, MD, discusses how the presentation of a patient with metastatic castration-resistant prostate cancer (mCRPC) involves evaluating factors such as disease progression despite androgen deprivation therapy, symptoms, prior treatments, and performance status to guide the selection of appropriate therapeutic strategies for managing this advanced disease state.

Evan Y. Yu, MD, discusses how adding chemotherapy to a doublet regimen for metastatic hormone-sensitive prostate cancer may be considered on an as-needed basis, particularly for patients with high disease burden or rapid progression, while carefully weighing the potential benefits and risks of intensifying therapy.

James J. Harding, MD, discusses how the initial findings from CheckMate 9DW inform the role of nivolumab plus ipilimumab (NIVO + IPI) in the first-line (1L) treatment landscape for unresectable hepatocellular carcinoma (uHCC), considering factors such as efficacy, safety, and patient characteristics (eg, age) when selecting between first-line systemic immunotherapy (IO) regimens.

Panelists discuss the PATINA study, examining the role of palbociclib in combination with letrozole as a first-line treatment for hormone receptor–positive, HER2-negative breast cancer, and its impact on progression-free survival.

Panelists discuss the findings from the DESTINY-Breast12 study, focusing on the efficacy and safety of trastuzumab deruxtecan in patients with HER2-low breast cancer and its potential to expand treatment options for this subgroup.

Panelists discuss the results and implications of the DESTINY-Breast06 study, highlighting the efficacy of trastuzumab deruxtecan in patients with HER2-positive breast cancer previously treated with multiple lines of therapy.

The panelist discusses how the treatment landscape for early-stage relapsed/refractory multiple myeloma (R/R MM) has evolved significantly with CAR T-cell therapies (idecabtagene vicleucel, ciltacabtagene autoleucel [ide-cel, cilta-cel]) and novel drug combinations. Treatment selection now considers prior therapies, patient characteristics, and response duration. For third-line chimeric antigen receptor (CAR) T after no prior CAR T use, cilta-cel shows favorable efficacy data with deeper, more durable responses than ide-cel, though both are viable options.

The panelist discusses how the patient had triplet therapy 6 years ago, which was the standard for myeloma treatment at the time. Since then, the patient has had a biochemical relapse, renal insufficiency, and moderate anemia, so he needs therapy but not immediate therapy.

A panelist discusses how, despite recent advances in relapsed/refractory follicular lymphoma treatment, important unmet needs are being addressed through ongoing trials while reflecting on proud accomplishments in the field and expressing enthusiasm for developments in the coming year.

Panelists discuss how the CEPHEUS trial demonstrates the comparative efficacy and safety of subcutaneous daratumumab combined with VRd vs VRd alone in patients with transplant-ineligible or transplant-deferred newly diagnosed multiple myeloma, highlighting key outcomes and clinical implications.

Experts examine the potential role of chimeric antigen receptor (CAR) T-cell therapy in chronic lymphocytic leukemia treatment, incorporating new evidence presented at the 66th American Society of Hematology Annual Meeting and Exposition 2024.

A panelist discusses adverse events with amivantamab and provides new recommendations for managing these skin-related events.

Thomas W. LeBlanc, MD, MA, discusses how existing challenges in treatment choices for low-risk myelodysplastic syndromes (LR-MDS) include limited access to newer therapies, patient-specific factors, and treatment sequencing complexities, and explores strategies to address these barriers, such as improving health care access, optimizing patient selection, and enhancing treatment guidelines.

Panelists discuss treatment options for patients ineligible for chimeric antigen receptor T-cell therapy in the second-line setting, focusing on the selection of new proteasome inhibitors and/or immune-mediated immunomodulatory drugs vs recycling combination regimens, and reviewing recent data from the APOLLO and IKEMA trials that support the use of combination therapies in relapsed/refractory multiple myeloma.

Panelists discuss the correlation between early and late toxicities observed in clinical practice for patients receiving chimeric antigen receptor T-cell (CAR T) therapy in early relapsed/refractory multiple myeloma and their perceptions of the latest International Myeloma Working Group Consensus Guidelines on response assessment and management of CAR T–related adverse events.

Evan Y. Yu, MD, discusses how community oncologists can critically weigh the evidence from studies on androgen deprivation therapy plus androgen receptor pathway inhibitors regimens by considering factors such as efficacy, safety, patient comorbidities, and treatment preferences, and how the collective trial results guide individualized treatment decision-making to optimize outcomes for patients with metastatic hormone-sensitive prostate cancer.

James J. Harding, MD, compares the responses observed with nivolumab plus ipilimumab (NIVO + IPI) therapy in the CheckMate 9DW trial to other first-line (1L) immunotherapy (IO) regimens for unresectable hepatocellular carcinoma (uHCC), including the HIMALAYA 5-year update (STRIDE) and the IMbrave150 trial (atezolizumab [ATEZO] + bevacizumab [BEV]), highlighting differences in efficacy and treatment outcomes.

Evan Y. Yu, MD, discusses how safety data for first-line androgen deprivation therapy plus androgen receptor pathway inhibitors (ARPI) regimens such as darolutamide, abiraterone, enzalutamide, and apalutamide reveal clinically relevant distinctions in their safety profiles, including the most common and challenging toxicities, incidence of grade 3 or higher adverse events, treatment discontinuations, and potential drug-drug interactions. He highlights key factors that influence treatment choice and disease management in patients with metastatic hormone-sensitive prostate cancer.
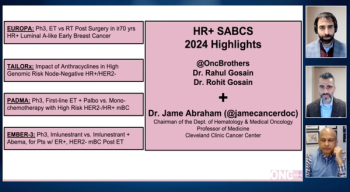
Panelists provide an overview of the EMBER-3 trial and its key findings.