
CAR T-Cell Therapy
Latest News
Latest Videos

More News

FDA updates CAR T-cell therapy labels, easing monitoring requirements and expanding access for eligible patients in oncology.

A new platform comprehensively profiles CAR T-cells during manufacturing, revealing phenotypic shifts. This allows for shorter timelines, better outcomes, and personalized therapies.
Lisocabtagene maraleucel led to promising responses in relapsed/refractory marginal zone lymphoma, offering a new option with manageable safety.

During a live event, Konstantinos Sdrimas, MD, and community oncologists discussed patient concerns over CAR T-cell therapy toxicity and how to coordinate with CAR T providers.

During a live event, Samuel M. Rubinstein, MD, discussed the outcomes from the KarMMa-3 trial and real-world patients receiving ide-cel in terms of bridging therapy, quality of life, and prior BCMA therapy.

During a live event, Konstantinos Sdrimas, MD, asked participants what community oncologists should consider when referring patients for CAR T-cell therapy.

During a live event, Samuel M. Rubinstein, MD, discussed the efficacy and safety outcomes from the KarMMa-3 trial.
In separate live virtual events, Sarah A. Holstein, MD, PhD, and Shashank Cingam, MD, discuss options for a patient with relapsed/refractory multiple myeloma and the use of chimeric antigen receptor (CAR) T-cell therapy.

Olalekan O Oluwole, MD, MBBS, discusses a study investigating shorter monitoring times post CAR T therapy.

The AERIAL trial will assess LEU011, which has MHRA Innovation Passport status, for solid tumors, a challenging area compared with hematologic cancers.

Frederick L. Locke, MD, discussed cema-cel's safety, efficacy, and potential for treating large B-cell lymphoma in earlier lines in the ALPHA trials.
During a live event, John L. Wagner, MD, moderated a discussion on when to refer patients for CAR T-cell therapy and what challenges the referral process poses.

During a Case-Based Roundtable® event, Natalie Galanina, MD, reviewed how outcomes have changed in patients with primary refractory or early relapsed DBLCL since the introduction of CAR T-cell therapy.

During a Case-Based Roundtable® event, Natalie Galanina, MD, discussed data from the ZUMA-7 and TRANSFORM trials in the first article of a 2-part series.
Poor physical performance in patients with non-Hodgkin lymphoma receiving CAR T-cell therapy was linked to worse survival and increased risk of neurotoxicity in a cohort study.
CAR T-cell therapy showed efficacy in relapsed large B-cell lymphoma across age groups, including patients 70 and 80 years or older.
Obecabtagene autoleucel improved survival and response durability in B-cell acute lymphoblastic leukemia patients with minimal residual disease–negative remission.
NKTR-255 with CD19 chimeric antigen receptor T-cell therapy improved 6-month complete response rates in relapsed/refractory large B-cell lymphoma.
Anakinra failed to reduce cytokine release syndrome or immune effector cell–associated neurotoxicity in patients with large B-cell lymphoma receiving liso-cel.
A phase 1 trial evaluating FSHR-targeting CAR T cells for patients with ovarian cancer has dosed the first patient in its third cohort.

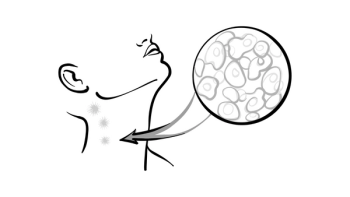
The advent of cellular therapies, such as chimeric antigen receptor T-cell therapy, has revolutionized the field of hematologic malignancies.

MT-303, a novel GPC3-targeting mRNA/lipid nanoparticle chimeric antigen receptor therapy, enhances cytokine-driven immune response and tumor cytotoxicity.
Doris K. Hansen, MD, discussed a comprehensive analysis of pretreatment biomarkers associated with outcomes in patients receiving idecabtagene vicleucel therapy

Second-line treatment with lisocabtagene maraleucel in relapsed/refractory LBCL has safety and efficacy outcomes similar to those in the trials supporting its FDA approval.

Outpatient lymphodepletion before brexucabtagene autoleucel was safe and showed similar non-relapse mortality compared with inpatient administration in B-ALL and MCL.





























